In-Depth Understanding of Lactose Intolerance in the UK
What is the prevalence of lactose intolerance among adults in the UK?

Can Adults Suddenly Become Lactose Intolerant? In the United Kingdom, lactose intolerance impacts a significant portion of the population, often linked to ancestral backgrounds associated with particular geographical regions, especially in Europe. Symptoms of lactose intolerance may emerge in adulthood due to various factors, including shifts in diet and overall gut health. Current estimates suggest that around 5-10% of adults are affected by this condition, as indicated by data from the NHS and local research, which provide valuable insights into its prevalence. It is essential to note that lactose intolerance does not uniformly affect all ethnic groups; individuals of Asian, African, and Mediterranean descent are at a considerably higher risk of developing this intolerance later in life, unlike those of Northern European heritage, who typically maintain sufficient lactase production throughout adulthood.
As understanding of lactose intolerance continues to evolve, an increasing number of individuals across the UK are actively searching for information on effective ways to manage their symptoms. Consequently, raising awareness about the prevalence and consequences of lactose intolerance has become vital for healthcare professionals and the general public alike, fostering a more informed approach to understanding and managing this condition.
Common causes of lactose intolerance in UK adults
In the UK, the onset of lactose intolerance may arise from inherent genetic predispositions or secondary factors, including gastrointestinal infections, which are more prevalent in specific population segments. Research conducted by Public Health England indicates that British adults with a familial history of lactose intolerance are more likely to develop symptoms. Furthermore, gastrointestinal infections like gastroenteritis can temporarily reduce lactase production, impairing the ability to digest lactose effectively.
Insights gleaned from health surveys in the UK reveal the distinctive presentation of lactose intolerance within the population. By identifying these common causes, individuals can more effectively assess their personal risk factors, promoting proactive health management and informed dietary choices tailored to their unique needs.
What are the available diagnostic methods for lactose intolerance in the UK?
Healthcare professionals throughout the United Kingdom employ a variety of diagnostic tests to accurately identify lactose intolerance, with the hydrogen breath test and the lactose tolerance test being the most commonly used methods. The hydrogen breath test measures hydrogen levels in the breath after the consumption of a lactose-containing beverage; elevated hydrogen levels suggest inadequate digestion of lactose. In contrast, the lactose tolerance test monitors blood glucose levels post-lactose ingestion; lower blood glucose levels after eating indicate lactose intolerance. This diagnostic methodology is standardised across NHS services, ensuring that patients seeking clarification regarding their symptoms have convenient access to these tests.
Patients can generally expect their general practitioners to recommend these tests based on the symptoms they report, ensuring a thorough diagnostic process. Obtaining an accurate diagnosis is imperative, as it lays the groundwork for developing effective management strategies tailored to the individual's specific needs.
How to make effective dietary adjustments for lactose intolerance in the UK

In the United Kingdom, managing lactose intolerance effectively often entails reducing dairy intake or incorporating lactase enzyme products. Many individuals have successfully integrated lactose-free alternatives, such as oat or almond milk, into their daily nutrition. The NHS provides extensive guidance on lactose-free options readily available in local supermarkets, assisting individuals in maintaining a balanced diet without experiencing discomfort.
For instance, traditional British recipes can be easily adapted using lactose-free ingredients; one may opt for lactose-free cheese in a classic cheese toastie or substitute cow's milk with almond milk in a delightful bread and butter pudding. By embracing these alternatives, individuals can ensure their nutritional needs are satisfied while still enjoying cherished British culinary traditions, ultimately enhancing their overall well-being and quality of life.
How Does Lactose Intolerance Develop in Adults in the UK?
What factors contribute to its onset in the UK?
In the United Kingdom, the onset of lactose intolerance in adults can be traced back to age-related declines in lactase production or post-viral effects, which are particularly common among middle-aged individuals. The lactase enzyme, essential for breaking down lactose, typically diminishes with age, resulting in challenges when digesting dairy products. Additionally, substantial dietary changes or prolonged consumption of high-dairy foods can worsen symptoms, emphasising the need for individuals to carefully monitor their dairy intake.
To effectively track symptoms, individuals might consider keeping a food diary that logs their dairy consumption alongside any related reactions. This awareness empowers individuals to make targeted dietary adjustments, reflecting common British eating patterns. For example, someone who enjoys the traditional fish and chips served with a creamy tartar sauce may need to evaluate their dairy intake alongside these beloved meals.
Why do genetics play a role in lactose intolerance in the UK?
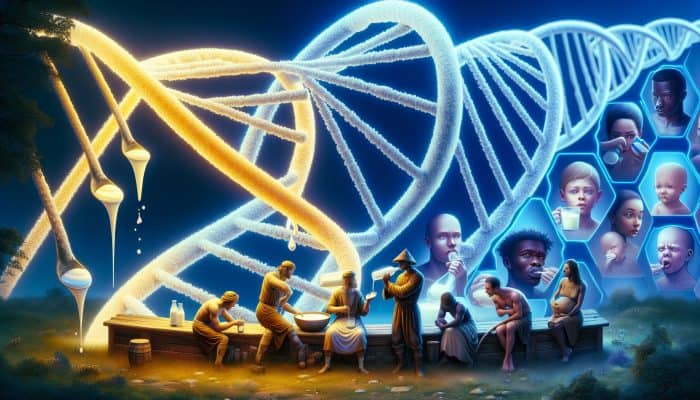
Genetic factors within the UK population significantly impact lactase production, with historical migration patterns playing a pivotal role. Certain populations, particularly those of Northern European descent, retain the ability to digest lactose well into adulthood. This stands in contrast to groups from regions where dairy farming was historically less prevalent, resulting in a gradual decline in lactase production after weaning.
Findings from genetic studies conducted in the UK illustrate how hereditary factors influence lactose tolerance levels among individuals. For those with a family history of lactose intolerance, recognising these genetic predispositions encourages proactive dietary modifications to alleviate discomfort and improve overall quality of life.
What lifestyle triggers can exacerbate lactose intolerance in British adults?
Certain lifestyle habits in the UK, such as high dairy consumption within traditional diets, can intensify symptoms of lactose intolerance. Many British individuals regularly indulge in dairy-rich foods, including tea with milk and cheese-laden dishes, which may provoke symptoms in those with lactose intolerance. Identifying these dietary triggers is crucial for effective management of the condition.
Key dietary habits that may worsen lactose intolerance among UK residents include:
- Consuming a daily cup of tea with milk.
- Indulging in cheese platters or rich cheese-based dishes.
- Enjoying creamy desserts such as Eton Mess or trifle.
- Using milk in cooking, particularly in sauces and soups.
By recognising these common eating patterns, individuals can make informed dietary choices that significantly enhance their health outcomes.
What is the role of secondary lactose intolerance in the UK?
In the United Kingdom, secondary lactose intolerance may develop as a result of gastrointestinal infections, surgical procedures, or conditions that compromise the intestinal lining, leading to a temporary reduction in lactase production. This situation is particularly relevant following episodes of gastroenteritis, during which the gut may need time to heal and restore its function. Recognising symptoms such as bloating, gas, and diarrhoea after consuming dairy products is essential, especially following gastrointestinal disturbances.
Seeking assistance from NHS services during recovery may involve dietary modifications, including the gradual reintroduction of dairy products or the use of lactose-free alternatives. Meticulously monitoring dietary habits during this recovery phase can facilitate a return to comfort while allowing the gut to regain balance and function effectively.
What preventive strategies can UK adults implement?
British adults can adopt several preventive measures to lower the risk of developing lactose intolerance, such as gradually decreasing dairy consumption or experimenting with lactose-free options. This proactive approach allows the digestive system to adapt to changes while ensuring adequate nutritional intake.
Incorporating fermented foods, such as yoghurt or kefir, into traditional UK diets may also promote gut health, owing to their robust probiotic content. Emphasising the importance of regular health check-ups through NHS services ensures that individuals remain informed about their digestive health and can take proactive steps towards maintaining overall well-being.
Insights from Experts on Sudden Onset of Lactose Intolerance in Adults
What sudden onset cases have been reported in the UK?
Experts in the United Kingdom have observed that sudden instances of lactose intolerance may arise following gastrointestinal illnesses, during which the gut's capacity to digest lactose can be temporarily impaired. Research indicates a surge in such cases after widespread occurrences of food poisoning or viral infections. This observation aligns with health trends in the UK, highlighting the importance of public education and awareness regarding this condition.
Understanding the relationship between gut health and lactose intolerance empowers individuals to seek timely medical advice when experiencing abrupt symptoms, rather than merely attributing discomfort to dietary choices or habits.
What professional advice is available for UK residents experiencing sudden symptoms?
In the UK, specialists recommend that individuals consult their general practitioners when they experience sudden lactose intolerance symptoms, particularly if these symptoms disrupt their daily routines. This advice is grounded in NICE guidelines advocating thorough evaluations of gastrointestinal symptoms. Real-world cases from UK patients underscore the significance of seeking professional guidance.
Upon consultation, healthcare providers typically suggest dietary adjustments or recommend diagnostic tests, such as the hydrogen breath test, to confirm lactose intolerance. This structured approach ensures effective symptom management, ultimately enhancing the quality of life for those affected.
What are the long-term implications of untreated lactose intolerance according to UK experts?
Experts in the UK highlight the potential nutritional risks linked to untreated lactose intolerance. If individuals continue to consume dairy products without acknowledging their intolerance, they may face deficiencies in essential nutrients, particularly calcium and vitamin D.
To support optimal bone health, UK experts propose several strategies:
- Incorporating fortified plant-based milks into the diet.
- Consuming leafy greens rich in calcium, such as kale.
- Choosing fortified breakfast cereals.
- Exploring lactose-free dairy options available in stores.
These strategies promote a balanced diet while addressing the nutritional needs of individuals with lactose intolerance, thereby enhancing their health and overall well-being.
What Are the Symptoms of Lactose Intolerance?
How do symptoms vary among UK adults?
The symptoms of lactose intolerance in the United Kingdom typically encompass <a href="https://limitsofstrategy.com/collagen-supplements-and-bloating-what-you-need-to-know/">bloating</a> and diarrhoea following dairy product consumption; however, they can manifest quite differently among individuals. Some may experience only mild discomfort, while others may endure significant gastrointestinal distress. This variability is crucial for understanding personal tolerance levels and making informed dietary decisions.
An analysis of UK health data indicates that the timing and severity of symptoms can depend on the amount of lactose consumed. For instance, certain individuals may tolerate small quantities of dairy, such as a splash of milk in their coffee, while larger servings, like a bowl of ice cream, could provoke noticeable symptoms.
What are the typical signs to watch for in the UK?
Common indicators of lactose intolerance in the UK may include abdominal pain following the consumption of foods such as milk in tea, a staple in numerous British households. Recognising patterns associated with specific foods can provide invaluable insights for individuals seeking to manage their condition effectively.
Expert analysis suggests utilising British health applications to efficiently monitor symptoms. Many of these applications allow users to log their food intake and corresponding reactions, aiding in identifying problematic foods and encouraging proactive dietary changes.
When should UK residents seek medical help?
If symptoms persist, UK residents are encouraged to consult NHS services to address their concerns. The urgency of seeking assistance may fluctuate based on symptom severity. For instance, ongoing diarrhoea or significant abdominal pain necessitates immediate attention to rule out other underlying gastrointestinal issues.
Real-world examples from UK clinics highlight the importance of early intervention. Patients who openly discuss their symptoms often receive tailored advice and management plans, significantly enhancing their quality of life and overall health.
Research-Backed Benefits of Managing Lactose Intolerance
What effective management strategies are available in the UK?
Research from UK studies indicates that enzyme supplements can greatly aid in managing lactose intolerance. These products enable individuals to digest lactose more comfortably, allowing for greater dietary flexibility and enjoyment.
Proven strategies for daily life include:
- Utilising UK-branded lactose-free milk for everyday consumption.
- Incorporating lactase enzyme pills before dairy intake.
- Exploring various lactose-free cheese options available in supermarkets.
- Trying plant-based alternatives in traditional British recipes to accommodate dietary needs.
By implementing these strategies, individuals can enhance their comfort while enjoying a diverse array of foods, ultimately improving their overall quality of life.
What benefits do dietary adjustments provide in the UK?
Adapting to a UK-friendly diet specifically tailored for lactose intolerance can significantly alleviate discomfort, as supported by local research. Those who successfully manage their symptoms often report increased energy levels and improved digestion.
Expert evaluations indicate that culturally relevant dietary modifications, such as substituting oat milk for cow's milk in traditional British recipes, can yield positive outcomes. These changes not only address lactose intolerance but also preserve the essence of cherished dishes, making them accessible for all.
How does treatment improve health outcomes in the UK?
UK research suggests that effective management of lactose intolerance leads to enhanced digestion and nutrient absorption. When individuals adhere to dietary recommendations and make informed choices, they typically experience fewer gastrointestinal issues and enjoy improved overall well-being.
Actionable steps derived from British dietary guidelines include increasing the intake of calcium-rich non-dairy foods and utilising fortified products to ensure a balanced diet. These strategies facilitate a smooth transition into a lactose-free lifestyle while effectively meeting nutritional requirements.
Why Might Lactose Intolerance Occur Suddenly?
What triggers sudden cases of lactose intolerance in the UK?
In the United Kingdom, sudden lactose intolerance can emerge from factors such as antibiotic use or heightened stress levels. Both can disrupt gut health, leading to unexpected and temporary changes in lactose tolerance. For instance, antibiotic treatment may disturb gut flora, impairing digestion and resulting in discomfort.
Examples from UK health reports illustrate instances where individuals develop symptoms after completing antibiotic courses, underscoring the need for awareness of these potential triggers. Recognising these connections enables patients to take preventive measures and adjust their diets as necessary.
How does age influence the sudden onset of lactose intolerance in the UK?
Age-related factors among UK adults can contribute to a sudden decline in lactase production, making lactose intolerance more prevalent as individuals grow older. The gradual decrease in lactase production is typically associated with the aging process, leading to unexpected symptoms in those who previously consumed dairy without issues.
Insights from British aging studies indicate that regular monitoring of dietary habits becomes increasingly crucial as individuals age. Taking a proactive approach by adjusting diets can help mitigate sudden-onset cases and promote overall digestive health.
What other potential causes are relevant in British contexts?
Environmental or medical factors specific to the UK, including certain medications, may contribute to the emergence of lactose intolerance. For example, individuals undergoing treatment for gastrointestinal disorders might experience decreased lactose tolerance.
Key risk factors identified through UK surveys include:
- Prolonged use of gastrointestinal medications that impact digestion.
- Recent surgeries affecting the digestive tract.
- Infections resulting in complications in gut health.
- Dietary changes stemming from significant life events.
Awareness of these factors can empower individuals to better understand their lactose tolerance and make informed dietary choices.
Prevention and Treatment Options in the UK
What preventive methods are available in the UK?
Preventive strategies in the United Kingdom involve gradually reducing dairy consumption, which can assist individuals in avoiding the sudden onset of lactose intolerance. This approach aligns with NHS recommendations, encouraging at-risk adults to be mindful of their dairy intake from an early stage.
Implementing small changes, such as opting for lactose-free products, can significantly enhance gut health. Raising awareness about lactose intolerance and its potential progression over time empowers individuals to take proactive control over their dietary choices.
What treatment options are available in the UK healthcare system?
The NHS offers various treatments to support individuals with lactose intolerance, including lactase pills that can be taken prior to consuming dairy products. This accessibility allows individuals to continue enjoying their favourite foods while minimising discomfort.
Real-life examples illustrate the benefits of these treatments; patients who utilise lactase supplements frequently report significantly improved experiences when consuming dairy products. This structured management approach fosters a positive relationship with food and nutrition, enhancing overall life satisfaction.
What are the long-term solutions for individuals in the UK?
Sustainable options available in the UK include consulting dietitians who can provide personalised strategies for maintaining a balanced lifestyle. This professional support proves invaluable for individuals navigating their dietary choices effectively.
By adhering to British nutritional standards, which emphasise variety in food selections, individuals can ensure their diets remain nutrient-rich while avoiding discomfort. Such solutions empower adults to embrace their dietary needs confidently and comfortably.
What educational resources and support groups are available in the UK?
Educational resources and support groups in the UK offer crucial guidance on managing lactose intolerance. These platforms equip individuals with the knowledge and community support necessary for effective management of their condition.
Online resources, helplines, and community networks provided by charities and the NHS facilitate the sharing of experiences and strategies for coping with lactose intolerance. These initiatives foster a sense of community and awareness, greatly enhancing the quality of life for many individuals affected by this condition.
Frequently Asked Questions about Lactose Intolerance
What are the main symptoms of lactose intolerance?
The primary symptoms encompass bloating, diarrhoea, gas, and abdominal cramps following the consumption of dairy products. These symptoms can vary in severity and may develop within a few hours post-ingestion.
Can lactose intolerance develop suddenly in adults?
Yes, lactose intolerance can manifest suddenly in adults, often triggered by gastrointestinal infections, stress, or dietary changes. Monitoring one’s dietary habits can assist individuals in recognising sudden shifts in their tolerance.
How is lactose intolerance diagnosed in the UK?
Diagnosis typically involves tests such as the hydrogen breath test or lactose tolerance test, which are readily available through NHS services. Consulting a GP is crucial for personalised assessment and guidance.
What dietary adjustments can help manage lactose intolerance effectively?
Reducing dairy consumption, opting for lactose-free products, and incorporating fermented foods like yoghurt into the diet can significantly aid in managing lactose intolerance. Seeking nutritional guidance can provide tailored support for individuals.
Is lactose intolerance the same for everyone?
No, symptoms and severity vary widely among individuals. Factors such as genetic background, age, and dietary habits significantly influence the presentation of lactose intolerance in each individual.
Can children also develop lactose intolerance?
While lactose intolerance is more prevalent in adults, children can develop it, particularly after experiencing gastrointestinal infections. Early identification and dietary modifications are crucial for effective management of symptoms.
Are there any medications available for lactose intolerance?
Yes, lactase enzyme supplements can be taken before consuming dairy to facilitate lactose digestion, enabling individuals to enjoy dairy products with minimal discomfort.
How can I determine if I am lactose intolerant?
If you experience symptoms like bloating or diarrhoea after consuming dairy, maintaining a food diary and consulting a healthcare professional can help ascertain whether you are lactose intolerant.
Do all dairy products cause symptoms for individuals with lactose intolerance?
Not necessarily; some individuals may tolerate small amounts of lactose, while others cannot consume any dairy. Understanding personal tolerance levels is essential for effective management of the condition.
Where can I find support for managing lactose intolerance?
Support groups, online communities, and NHS resources provide guidance and shared experiences for individuals managing lactose intolerance, helping them navigate their dietary choices effectively.
Connect with us on Facebook!
This Article Was First Found On https://bloodtest.co.uk
The Article Lactose Intolerance: Can Adults Develop It Suddenly? Was Found On https://limitsofstrategy.com
The Article Lactose Intolerance in Adults: Can It Develop Suddenly? found first on https://electroquench.com

